Polycystic Kidney Disease Treatment is essential for people who have this inherited condition. While there is no complete cure, effective management options can help slow down the disease and improve the quality of life. If you or a loved one have been diagnosed with PKD, knowing about the different treatment options available can help you make informed decisions. In this blog, we will cover everything you need to know about Polycystic Kidney Disease Treatment, management approaches, and ways to handle this condition.
What is Polycystic Kidney Disease (PKD)?
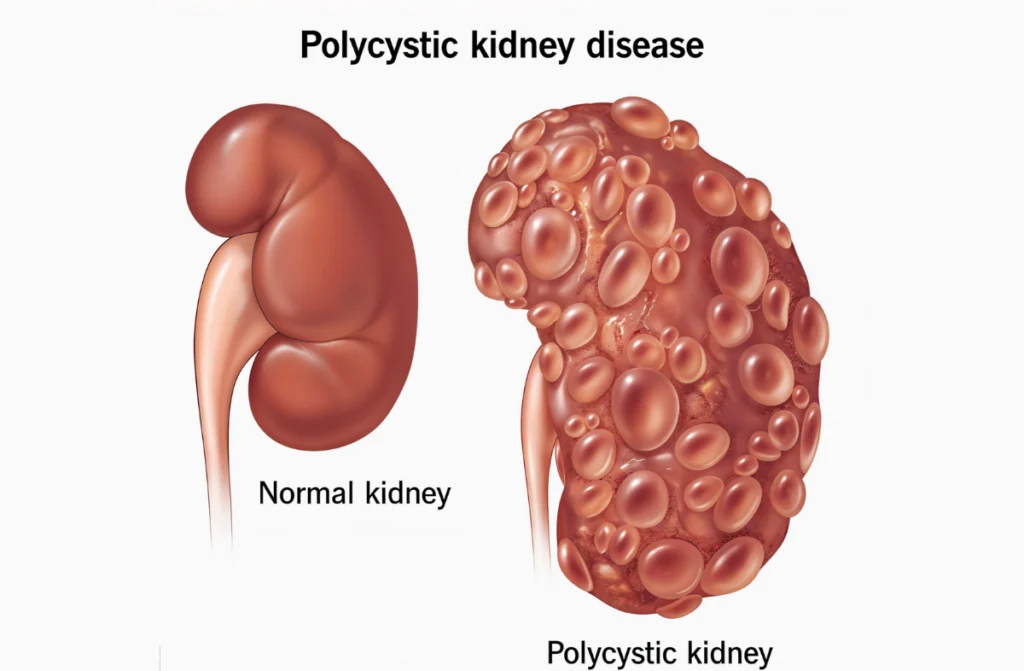
Polycystic Kidney Disease (PKD) is a genetic disorder where fluid-filled cysts grow on the kidneys. These cysts can multiply and grow large over time, making the kidneys swell and lose function. PKD affects kidney function and can lead to kidney failure if not managed properly.
Types of PKD:
- Autosomal Dominant PKD (ADPKD): More common, symptoms usually appear between the ages of 30 and 40.
- Autosomal Recessive PKD (ARPKD): Rare, often detected in infants or children.
Managing PKD is critical, and effective Polycystic Kidney Disease Treatment can slow down the progression.
PKD Treatment Approaches
1. Managing Symptoms
- High Blood Pressure Control: Medications like ACE inhibitors and ARBs can help.
- Pain Relief: Painkillers can ease the discomfort caused by cyst growth.
- Infections: Antibiotics are used to treat kidney or bladder infections.
2. Dialysis
- For those with advanced PKD, dialysis helps remove waste from the blood when kidneys can’t.
3. Polycystic Kidney Disease Transplant Success Rate
- Kidney Transplant: A viable option for end-stage kidney failure. The polycystic kidney disease transplant success rate is high, offering a new chance at life for many patients.
By focusing on these approaches, patients can effectively manage their condition and slow its progression.
Types of Polycystic Kidney Disease (PKD)
Polycystic Kidney Disease Treatment varies depending on the type of PKD a person has. Knowing the type of PKD can help determine the best way to manage it.
- Autosomal Dominant PKD (ADPKD):
- Most common type, affecting adults.
- Symptoms typically show up in adulthood, such as high blood pressure, kidney pain, and urinary tract infections.
- Autosomal Recessive PKD (ARPKD):
- Affects infants and children.
- Can lead to serious complications early in life, including liver problems.
Early diagnosis and treatment are essential for both types to avoid complications and improve outcomes.
Signs and Symptoms of PKD
Recognizing the symptoms early can lead to better Polycystic Kidney Disease Treatment. Here are some common signs:
- High Blood Pressure: Often the first sign of PKD.
- Back or Side Pain: Due to the enlarged kidneys.
- Frequent Urinary Tract Infections (UTIs).
- Blood in Urine: A sign that cysts have ruptured.
- Kidney Stones.
If you experience any of these symptoms, seek medical help immediately for timely diagnosis and management.
Causes of PKD
Polycystic Kidney Disease is caused by genetic mutations. Here’s what you need to know:
- Inherited Genes: PKD is passed down from one or both parents.
- Mutations: Changes in the PKD1, PKD2, or PKHD1 genes lead to the formation of kidney cysts.
Understanding the causes helps in early diagnosis and better Polycystic Kidney Disease Treatment. If you have a family history of PKD, it’s a good idea to get screened.
Diagnosis of PKD
Early diagnosis is key to successful Polycystic Kidney Disease Treatment. Doctors use different methods to detect PKD:
- Ultrasound: Detects cysts in the kidneys.
- CT Scan: Provides detailed images of the kidneys.
- MRI: Shows the size and number of cysts.
- Genetic Testing: Helps confirm PKD, especially if there’s a family history.
If diagnosed early, Polycystic Kidney Disease management can help reduce complications and improve your quality of life.
Prevention
While you can’t prevent PKD since it’s genetic, you can prevent complications with the right Polycystic Kidney Disease Treatment plan. Here are a few tips:
- Control Blood Pressure: Maintain a healthy diet low in salt and processed foods.
- Stay Hydrated: Drink enough water to support kidney function.
- Exercise Regularly: Helps with overall health and weight management.
- Avoid Smoking and Alcohol: Both can damage kidney health.
By following these steps, you can improve your health and slow the progression of PKD.
Latest Treatment for Polycystic Kidney Disease
Medical research is advancing rapidly, offering new hope for patients.
Latest Treatment Options:
- Tolvaptan: A medication that slows down cyst growth and protects kidney function.
- Gene Therapy: Experimental treatments targeting the genetic cause of PKD.
- New Pain Management Methods: Non-invasive ways to manage kidney pain.
These latest treatment for polycystic kidney disease options are improving outcomes for patients with PKD. Discuss these with your doctor to see if they are right for you.
Polycystic Kidney Disease Management
Managing PKD involves a combination of lifestyle changes and medical care. Here’s what you can do:
- Follow a Healthy Diet: Low-sodium, low-fat foods.
- Regular Check-ups: Monitor kidney function regularly.
- Stay Active: Exercise helps control blood pressure and improves overall health.
Effective Polycystic Kidney Disease management can slow the progression of the disease and help you lead a normal life.
Conclusion
Polycystic Kidney Disease Treatment is essential for improving quality of life and slowing the progression of the disease. With the right management, advanced treatments, and proper medical care, people with PKD can live longer, healthier lives. If you or a loved one is struggling with PKD, don’t hesitate to seek help.
