Hypertensive nephropathy treatment is important for people who suffer from kidney damage caused by high blood pressure. This condition can worsen over time if not properly treated. Managing high blood pressure and protecting the kidneys are the main goals of treatment. In this blog, we will cover what hypertensive nephropathy is, its symptoms, stages, and how it can be treated. We will also discuss related issues like hypertension after kidney transplant and the best hypertension medication for kidney disease.
What is Hypertensive Nephrosclerosis?
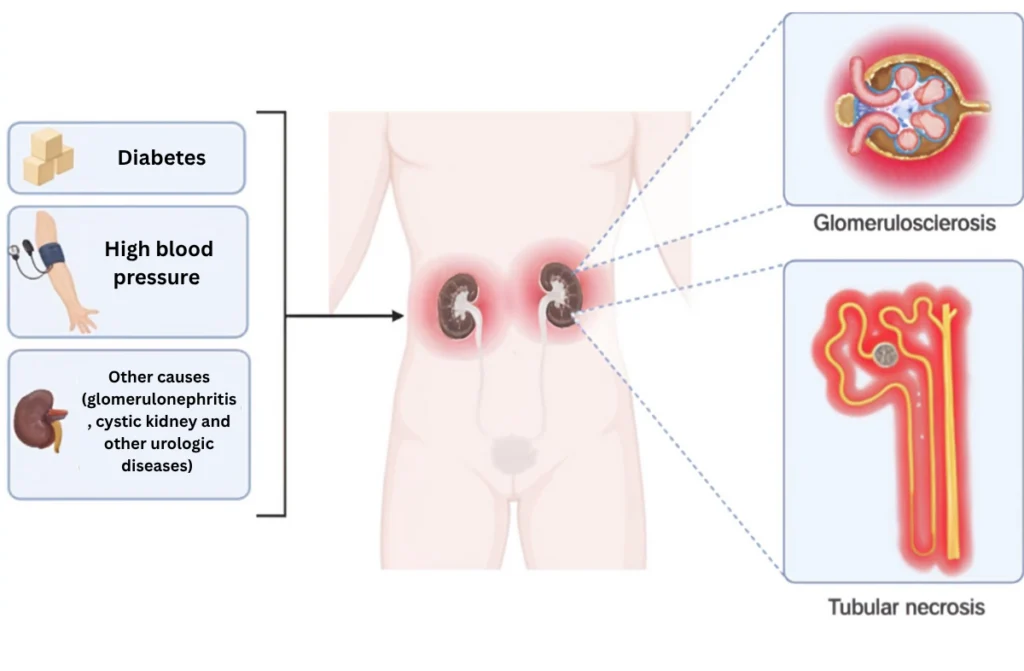
Hypertensive nephrosclerosis is a type of kidney damage caused by long-term high blood pressure. When blood pressure stays high for a long time, it damages the small blood vessels in the kidneys. This makes the kidneys less effective at filtering waste and extra fluid from the blood. If left untreated, it can lead to chronic kidney disease (CKD) or kidney failure.
Key Points to Understand:
- High Blood Pressure: The main cause of hypertensive nephropathy.
- Kidney Damage: Over time, the kidneys can become scarred.
- Treatment: Effective hypertensive nephropathy treatment focuses on lowering blood pressure and protecting kidney function.
Early diagnosis and proper treatment can slow down kidney damage and help maintain kidney health.
Comprehensive Treatment for Hypertensive Nephropathy
Effective hypertensive nephropathy treatment focuses on controlling blood pressure and protecting the kidneys. Here are some key approaches:
1. Medications
- ACE Inhibitors: These drugs help lower blood pressure and protect kidney function.
- ARBs (Angiotensin II Receptor Blockers): Another class of drugs that helps manage high blood pressure.
- Best Hypertension Medication for Kidney Disease: Your doctor will choose the best medication based on your condition.
2. Lifestyle Changes
- Healthy Diet: Low in salt and fat.
- Exercise: eRegular physical activity helps control blood pressure.
- No Smoking: Smoking damages blood vessels and kidneys.
Proper hypertensive nephropathy treatment can slow the progression of kidney damage and improve quality of life.
Symptoms of Hypertensive Nephropathy
It’s important to recognize the symptoms early to get proper hypertensive nephropathy treatment. Here are some common symptoms:
- High Blood Pressure: Uncontrolled or resistant high blood pressure.
- Swelling (Edema): Especially in the legs, feet, or hands.
- Fatigue: Feeling tired even after resting.
- Frequent Urination: Especially at night.
- Headaches: Often due to high blood pressure.
If you notice any of these symptoms, see a doctor as soon as possible. Early hypertensive nephropathy treatment can help prevent serious complications.
Stages of Hypertensive Nephropathy
It depends on the stage of kidney damage. The stages range from mild to severe kidney damage.
1. Stage 1: Early Damage
- Slight decrease in kidney function.
- High blood pressure is present.
- Treatment focuses on blood pressure control.
2. Stage 2: Mild to Moderate Damage
- Kidney function continues to decline.
- Protein may be present in the urine.
- Medication and lifestyle changes are key treatments.
3. Stage 3: Moderate to Severe Damage
- Significant drop in kidney function.
- More symptoms like swelling and fatigue.
- Dialysis may be considered.
4. Stage 4 & 5: Severe Kidney Damage / Kidney Failure
- Kidney function is very low.
- Dialysis or kidney transplant may be needed.
Knowing the stage of your condition helps in choosing the right hypertensive nephropathy treatment.
Hypertension After Kidney Transplant
Some patients experience hypertension after kidney transplant. This can happen due to:
- Side Effects of Medications: Some drugs used after a transplant can raise blood pressure.
- Underlying Conditions: Existing heart or blood vessel issues.
- Donor Kidney Issues: The health of the donor kidney can affect blood pressure.
Managing Hypertension After Kidney Transplant
- Medications: Adjusting your medication can help control blood pressure.
- Healthy Lifestyle: Diet, exercise, and regular check-ups are key.
Managing hypertension after kidney transplant is crucial to protect the new kidney and your overall health.
Best Hypertension Medication for Kidney Disease
Choosing the best hypertension medication for kidney disease is important for effective hypertensive nephropathy treatment. Common options include:
- ACE Inhibitors (e.g., Lisinopril): These drugs lower blood pressure and protect kidney function.
- ARBs (e.g., Losartan): Similar to ACE inhibitors but with fewer side effects.
- Calcium Channel Blockers: Help relax blood vessels.
Factors to Consider:
- Kidney Function: Some medications may not be suitable if kidney function is very low.
- Side Effects: Your doctor will help choose the best option for you.
Finding the best hypertension medication for kidney disease can make a big difference in your treatment.
Prevention of Hypertensive Nephropathy
Prevention is better than cure. Here are some tips:
- Monitor Blood Pressure: Regularly check your blood pressure and keep it under control.
- Healthy Diet: Eat low-sodium, balanced meals.
- Exercise: Stay active with at least 30 minutes of exercise per day.
- Avoid Smoking: Smoking damages blood vessels and kidneys.
- Regular Check-ups: Early detection of high blood pressure can prevent kidney damage.
By following these steps, you can reduce your risk of hypertensive nephropathy.
Diagnosis of Hypertensive Nephropathy
Early diagnosis helps in effective hypertensive nephropathy treatment. Doctors use these tests:
- Blood Pressure Measurement: High blood pressure can be a sign.
- Urine Test: Checks for protein or blood in the urine.
- Blood Test: Measures kidney function.
- Imaging Tests: Ultrasound or CT scan to check kidney structure.
If diagnosed early, proper hypertensive nephropathy treatment can help protect your kidneys.
Conclusion
Hypertensive nephropathy treatment is key to protecting your kidneys and managing high blood pressure. Whether you need medication, lifestyle changes, or advanced care, getting the right treatment can make a huge difference. If you are dealing with hypertension or kidney issues, don’t wait.
